Former Georgia State Insurance Commissioner Pleads Guilty to Healthcare Fraud Conspiracy

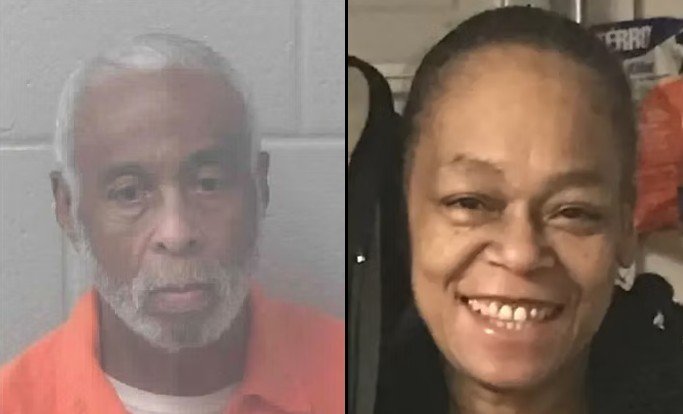
John W. Oxendine, the former Georgia State Insurance Commissioner, has pleaded guilty today to conspiracy to commit health care fraud. The plea follows allegations of orchestrating a scheme with a co-conspirator involving unnecessary medical tests, for which they received substantial kickbacks.
U.S. Attorney Ryan K. Buchanan highlighted Oxendine’s breach of trust, stating, “John Oxendine, as the former state-wide insurance commissioner, knew the importance of honest dealings between doctors and insurance companies. But for personal profit, he willfully conspired with a physician to order hundreds of unnecessary lab tests, costing hundreds of thousands of dollars. He will now be held accountable for violating the public’s trust.”
The scheme involved referring unnecessary medical tests to a lab company in Texas in exchange for kickbacks amounting to hundreds of thousands of dollars, according to FBI Atlanta’s Special Agent in Charge, Keri Farley. Farley emphasized the negative impact of such actions on healthcare costs and patient trust.
Special Agent in Charge Tamala E. Miles of the U.S. Department of Health and Human Services Office of Inspector General (HHS-OIG) underscored the risk such kickback schemes pose to federal healthcare programs, stating, “Individuals who participate in kickback schemes risk undermining the integrity of federal health care programs.”
Furthermore, Darrin K. Jones, Special Agent-in-Charge of the Department of Defense Office of Inspector General, emphasized the importance of deterring fraud that affects vital healthcare systems such as TRICARE.
According to U.S. Attorney Buchanan, Oxendine collaborated with Dr. Jeffrey Gallups and others to submit fraudulent insurance claims for medically unnecessary tests, including Pharmacogenetic, Molecular Genetic, and Toxicology testing. The scheme involved pressuring physicians associated with Dr. Gallups’s ENT practice to order these tests from a lab company in Texas.
Oxendine also utilized his influence to pressure doctors into ordering the unnecessary tests, as revealed by his presentation at the Ritz Carlton in Buckhead.
The fraudulent claims amounted to over $2.5 million, leading to almost $700,000 in payments from insurance companies to the lab company. Oxendine and Dr. Gallups received kickbacks totaling $260,000. Some patients were also charged exorbitant amounts for these unnecessary tests.
To conceal the kickback payments, Oxendine arranged for payments to be made to his insurance consulting business. He then used a portion of this money to pay debts for Dr. Gallups, including a charitable contribution and attorney’s fees.
Oxendine’s attempts to cover up the scheme included instructing Dr. Gallups to lie about the nature of payments and falsely denying involvement with the lab company when questioned by federal agents and during media inquiries.
Sentencing for Oxendine is scheduled for July 12, 2024, before U.S. District Judge Steve C. Jones. The investigation into this case is a collaborative effort involving the Federal Bureau of Investigation, the U.S. Department of Health and Human Services Office of Inspector General, and the Defense Criminal Investigative Service.